By Hope Kameta, Founder-Triphasic Health Alliance
Pandemics are not rare, unpredictable flukes, they are inevitable outcomes of complex biological, ecological and system interactions. In the last two decades alone, the world has faced SARS in 2002, H1N1 in 2009, MERS in 2012, several Ebola outbreaks, the Zika virus in 2015, and most recently, COVID-19. While each outbreak had unique features, common threads connect them: zoonotic origins, weak early detection systems, fragmented global responses, and unequal access to life-saving interventions. As the world recovers from the devastating impacts of COVID-19, attention has turned to a pressing question: what will the next pandemic look like, and how can we be better prepared?
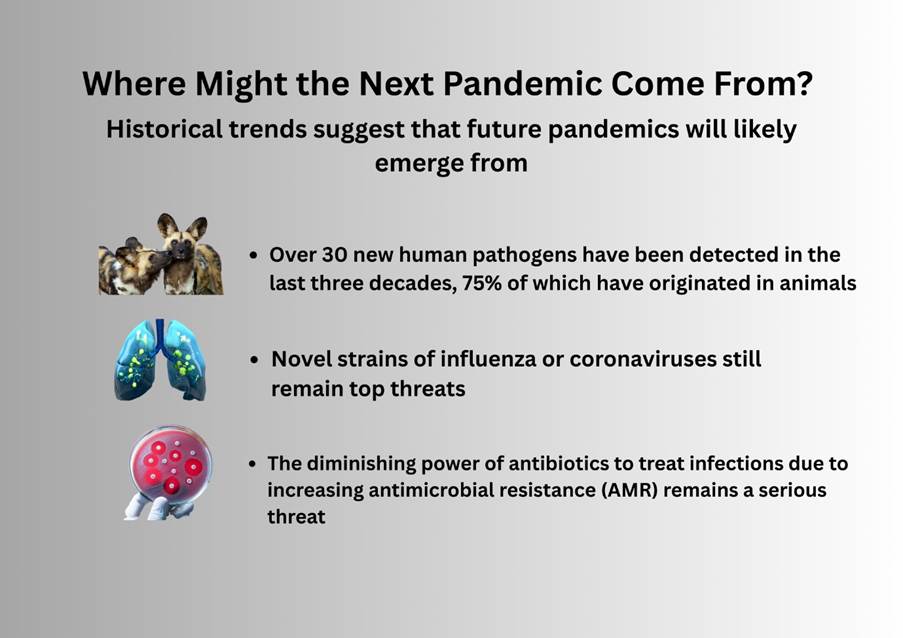
Historical trends suggest that future pandemics will likely emerge from zoonotic spillovers, where diseases jump from animals to humans. Over 70% of emerging infectious diseases originate this way, often facilitated by deforestation, habitat encroachment, and increased interaction between wildlife and human populations. Respiratory viruses remain one of the most concerning threats due to their ease of transmission, and novel strains of influenza or coronaviruses are particularly high on the risk radar.
Meanwhile, antimicrobial resistance (AMR) poses a slower, but equally dangerous, long-term pandemic risk. Climate change, rapid urbanization, and increased global mobility further complicate the landscape, creating ideal conditions for the emergence and spread of novel pathogens.
When COVID-19 erupted, global systems were caught off guard. Many countries responded independently, hoarding supplies, closing borders, and prioritizing national interests over collective security. These actions highlighted systemic failures in early outbreak detection, rapid response coordination, equitable access to medical countermeasures, and communication. The pandemic revealed that while we possess the scientific knowledge and technology to combat such threats, we lack the unified systems and political will to respond effectively and equitably.
To address these weaknesses, the World Health Organization (WHO) and its Member States have adopted the Pandemic Agreement, an international accord aimed at improving global readiness, cooperation, and equity in the face of future pandemics. This agreement is envisioned as a tool for fostering collaboration across countries, sectors, and agencies. It emphasizes a “whole-of-government and whole-of-society” approach, encouraging public-private partnerships, involvement of civil society, and inter-agency coordination to ensure that responses are comprehensive and inclusive.
One of the core goals of the Pandemic Agreement is to ensure equitable access to health tools. During the COVID-19 pandemic, vaccine nationalism and unequal distribution of diagnostics and treatments left many low-income countries behind. The agreement seeks to establish systems for fair distribution, promote technology transfer, and support local production of medical tools, ensuring that no country is left vulnerable in times of crisis. It also supports stronger global surveillance networks, enabling faster sharing of genetic data and pathogen samples to identify and respond to emerging threats more swiftly.
Additionally, the agreement encourages countries to strengthen their own health systems through investments in workforce development, laboratory infrastructure, supply chains, and emergency preparedness. This capacity-building is essential, as no global response can succeed without strong national systems forming the foundation. The agreement also includes provisions for accountability, with mechanisms to monitor progress, assess compliance, and evaluate effectiveness. These systems of shared responsibility aim to prevent backsliding and ensure ongoing commitment.
Although the WHO Pandemic Agreement cannot prevent pandemics from occurring, it serves as a global insurance policy, one that emphasizes preparedness over panic and proactive collaboration over fragmented reaction. It is not a tool for centralized control or loss of national sovereignty. Instead, it offers a framework for voluntary cooperation, ensuring that countries can work together while maintaining autonomy over their health policies. It provides a much-needed shift from the reactive, unequal responses of the past to a forward-looking, collective strategy for global health security.
The COVID-19 pandemic was a seismic event that disrupted lives, economies, and health systems around the world. It underscored the reality that global health is interconnected, and that the failure of one system can quickly affect all others. With the lessons from COVID-19 still fresh, the international community has a rare window of opportunity to act. By adopting and implementing the WHO Pandemic Agreement, countries can strengthen the world’s preparedness and response capacity, building a more resilient and equitable future.
The next pandemic is a matter of when, not if. Whether we meet it disjointed and unprepared or united and ready depends on the choices we make today. The WHO Pandemic Agreement offers the foundation for a stronger global response. What we do with it will shape the course of the next global health emergency.
Leave a comment